Continence Assessment Forms for a Child who has not yet been toilet trained
The form below not only suggests which questions should be asked as part of a comprehensive continence assessment, but also explains why the questions should be asked and what the answers might mean. It signposts sources of further information and other useful tools.
The assessment form can therefore be used both to document a child’s bladder and bowel behaviour and as a teaching aid.
Use this form to assess a child who has not yet been toilet trained. Some children with complex additional needs may never achieve continence. However, even children with significant learning, mobility or communication difficulties can achieve a good level of continence. Every child has the right to be helped to achieve their best possible level and to maintain their dignity.
Even if a child is unable to achieve full continence, a healthy bladder and healthy bowels should be promoted at all times. Constipation is very common in children with additional needs, and is often overlooked as their bowel problems are incorrectly attributed to their learning disability. Constipation may result in frequent, loose bowel actions (overflow soiling) which can cause sore skin. The full rectum and colon also occupy the space required for the bladder to expand, resulting in frequent small voids, and placing the child at risk of Urinary Tract Infection (UTI) as bladder emptying is impaired.
NO child should ever be provided with nappies, pull-ups or pads without a full continence assessment to identify any bladder or bowel problems and to consider their toilet training potential.
If a child with additional needs is toilet trained please assess using the Continence Assessment Form - Child that has been toilet trained.
(**IMPORTANT** This word version must be used with the ERIC logo intact, OR if it is amended in any way after downloading, the ERIC logo needs to be removed and an acknowledgement of ERIC as the original author added saying 'Adapted from the ERIC original resource'.**)
| Bowels | For any continence assessment, the starting point must be the bowels. This is because of the very close relationship between bladder and bowels; wetting can be entirely caused by constipation! |
| Frequency of bowel actions:
____________ times a day/week |
The normal range is anything from three times a day to three times a week. However, most children poo every day. Children should be encouraged to poo at least every other day.
Record bowel actions on the Bladder/Bowel Assessment Chart. If a longer record is required use the Poo Diary. If child is pooing more frequently consider:
Is this constipation and/or overflow? See Advice for Children with Constipation for explanation. |
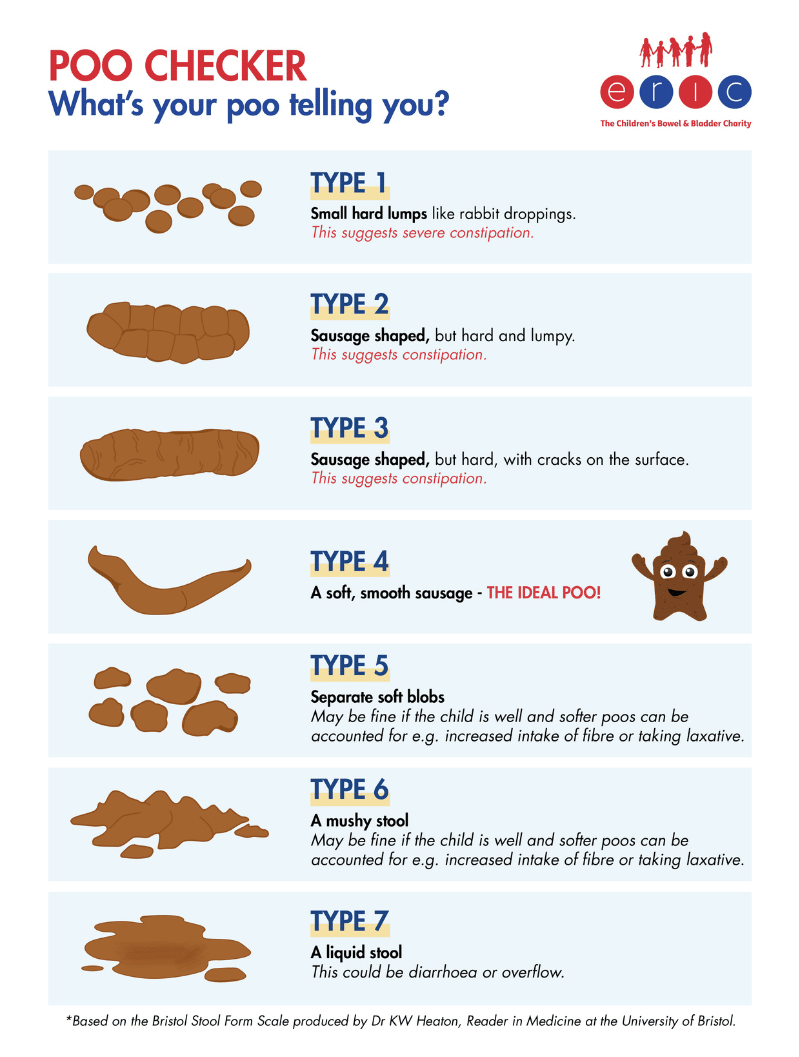
| Stool Type
1 2 3 4 5 6 7 |
Types 1-3 all suggest constipation in a child, with Type 1 being the most severe. Type 4 is the ideal poo! Types 5 & 6 may be fine if the child is well and softer stools can be accounted for (e.g. increased intake of fibre, taking laxatives). Type 7 could be diarrhoea or overflow. If child has persistent loose stools consider:
Is this overflow caused by constipation? See Advice for Children with Constipation for explanation. |
| Any soiling?
Yes / No |
If the child is soiling always suspect constipation – remember almost all childhood soiling is caused by functional constipation! In a child who is not continent of faeces, soiling may be identified as ‘leaking’ of faeces between bowel actions. The child may not seem to evacuate a complete bowel action. When wiping their bottom, there may be constant leakage noted; this suggests a full rectum which is a definite indicator of constipation. |
| What protection does the child wear?
Pants / pad in pants / nappy / pull-up |
Consider if child is eligible for products from Continence Service. See Flowchart - Child with Additional Needs.
NB Additional needs can include organic underlying bladder/bowel conditions such as neuropathic bladder/bowels, ano-rectal anomalies, cloacal anomalies and significant learning disabilities. |
| Does the child use the potty / toilet / neither?
Is there a regular toileting programme in place? Yes / No |
|
| Does the child pass LARGE stools / large quantity of stool all at once?
Yes / No |
In order to pass a large amount of stool at once, the stool must have accumulated over a period of time. This represents constipation. The accumulated stool will stretch the rectum; if this is allowed to persist there will be a loss of rectal tone which will diminish the sensation of the need to poo. |
| Any abdominal pain and/or pain on defaecation?
Yes / No |
This could be caused by constipation. |
| Any abdominal distension?
Yes / No |
This could be caused by constipation. Note, the presence of gross abdominal distension represents a red flag finding (NICE Guidelines). |
| Any anorexia / nausea / vomiting / faltering growth?
Yes / No |
This could be caused by constipation. Note, the presence of faltering growth represents a red flag finding (NICE Guidelines). |
| Any other associated behaviour – straining / stool withholding / toilet avoidance / passing stools at night?
Yes / No |
This could be caused by constipation. |
| The child does not have to display all these symptoms to be diagnosed with constipation. See NICE Guideline CG99 – Constipation in children and young people - two or more findings indicate constipation. | |
| If constipation is indicated follow Flowchart for Constipation. | |
| Has child been seen by GP/Paediatrician for physical examination to rule out underlying organic cause – ‘red flags’?
Yes / No / Referred |
See NICE Guideline CG99 – Constipation in children and young people. Remember the child may have e.g. a very subtle spinal anomaly – constipation may be the only presenting symptom. The physical examination should not be omitted. |
| Daytime Bladders | Remember to always assess the bowels first. This is because of the very close relationship between bladder and bowels; wetting can be entirely caused by constipation! Therefore constipation is a significant obstacle to toilet training. |
| Frequency of voids:
_______________ times a day |
The normal range is considered to be 4–7 voids per day. Voiding frequency should be assessed in conjunction with an assessment of fluid intake – infrequent voids can of course be caused by an inadequate fluid intake, and vice versa! An assessment tool such as the Bladder/Bowel Assessment Chart should therefore be used. If the child is voiding more than once an hour check for constipation/UTI. Review fluid intake – concentrated urine can irritate the bladder. If child is over 5 years old and frequent voids persist in the absence of constipation/UTI and the child has an adequate fluid intake, consider treatment for overactive bladder. |
| Voiding behaviour:
Any hesitancy? Yes / No Any straining to initiate void? Yes / No Is stream weak/interrupted? Yes / No |
Any of these voiding behaviours could suggest Dysfunctional voiding. A weak stream could also be indicative of bladder outflow obstruction and should be investigated.
Advise time without nappy to allow observation of stream. |
| History of Urinary Tract Infection (UTI)
Yes / No Number of UTIs in the last year _________ Current UTI suspected? Yes / No Urinalysis performed? Yes / No Result _______________________________ Specimen sent? Yes / No Result _______________________________ |
Symptoms may include:
Remember, children may not display all these symptoms. Check for asymptomatic bacteriuria if the child is well but has frequency / urgency / wetting. |
| If UTI confirmed see NICE Guideline CG54 – Urinary Tract Infections in under 16s. | |
| What protection does the child wear?
Pants / pad in pads / nappy / pull-up |
Consider if child is eligible for products from Continence Service. See Flowchart - Child with Additional Needs.
NB Additional needs can include organic underlying bladder/bowel conditions such as neuropathic bladder/bowels, ano-rectal anomalies, cloacal anomalies and significant learning disabilities. |
| What are the child’s usual drinks/feeds?
__________________________________ |
Caffeine can cause bladder disturbance and should always be avoided. Blackcurrant / orange / artificial colourings / flavourings / sweeteners / carbonated drinks are all bladder irritants for some people – so should be trialled to assess effect on individual child. |
| How many drinks/feeds does the child have every day?
_____________________ Are drinks/feeds evenly spread throughout the day? Yes / No Average daily fluid intake?__________mls |
We all need to have at least 6-8 cups of water-based fluid every day, spread evenly over the day. The cup size should be appropriate to the child's size e.g. about 200mls for a 7 year old, 250mls for an 11 year old. If fluid intake is inappropriate in type and/or quantity - correct, then re-assess bladder.
See Advice for Children with Daytime Bladder Problems for more information. |
| If daytime bladder problems are indicated follow Flowchart for Daytime Bladders. | |
| Has child been seen by GP/Paediatrician for physical examination to rule out underlying organic cause?
Yes / No / Referred |
If bladder/bowel assessment demonstrates frequent, small volume voids or there is a history of UTI a physical examination should be performed. Remember the child may have e.g. a very subtle spinal/urological anomaly – small, frequent voids may be the only presenting symptom. The physical examination should not be omitted. |
| Night Time Bladders | If the child is not continent during the day it is entirely normal to be wet at night. If however they develop night time wetting as a new symptom it should be investigated. |
| Is the child occasionally or regularly wet at night?
Yes / No If yes – continue assessment below. |
|
| Is the wetting:
Primary – the child has never been dry at night for a 6 month period? Secondary – the child has been dry at night for at least 6 months prior to this episode? |
If primary and the child is not continent during the day no further assessment or action required.
If secondary, assess for a systemic cause or trigger or comorbidities, e.g. UTI, constipation, Diabetes mellitus, psychosocial situation, neurological cause. |
This assessment complies with these national and international standard documents:
- NICE Guideline CG99 – Constipation in children and young people
- NICE Guideline CG111 – Bedwetting in under 19s
- International Children's Continence Society (ICCS) Terminology, Standardisation document, Assessment of daytime wetting (available through membership of the ICCS website)
Upcoming dates
Share this page